In our constant efforts to improve the Follicular Unit Extraction (FUE) experience, we’ve figured out a way to perform FUE without shaving the donor area! We call this procedure a mini-FUE (mFUE). One of the great drawbacks to FUE has been the social disruptions that shaving the side and back of the head causes in people undergoing this procedure. Many patients choose to stay away from social engagements until the hair grows out (enough to hide the donor wounds made by the FUE technique on the donor area). Having long hair in front and on the top of the head with a shaved back of the head draws attention, and people wonder why you have this crazy haircut. It is hard to keep a secret.
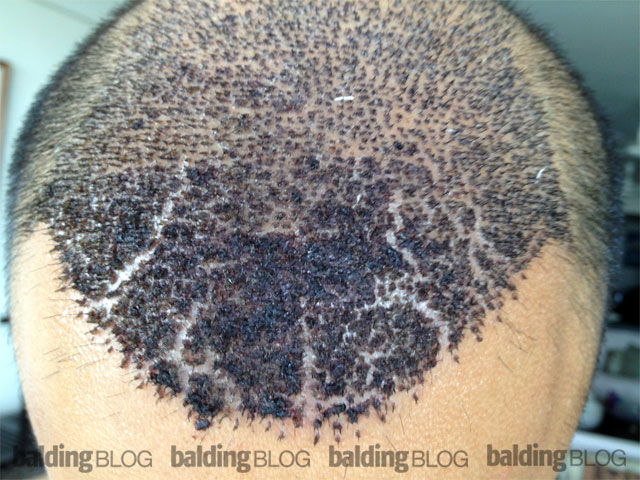
We have developed and tested the use of FUE harvesting without shaving the donor area, which allows us to go directly into the donor area where we extract the FUE grafts. We advise the patient to wash the back of their head the next morning, then combing it, apply whatever products to hold the hair, and then go on with your day. With FUE, there are no restrictions with regard to exercise or lifting weights within 36 hours of the procedure and if a patient wants to run a marathon, we will not stop them.
At this time, we are limiting the size of these sessions to no more than 300 grafts per session and are introducing this technique at a cost of $3000. With careful planning, the patient can come back as often as they wish, adding 300 grafts each time. This technique works well for people needing small amounts of hair, for example: (a) advancing the hairline, (b) filling in a hairline, (c) filling in areas where further hair loss progressed, (d) touch-up as needed. We do not recommend large session, long hair FUE procedures at this time.
Call our office today at 800-NEW-HAIR to arrange a consultation!

 There is a question arising out of the hair transplant community which is becoming polarized and lining up for a fight: Which is better, FUT (Follicular Unit Transplant with Strip) or FUE (Follicular Unit Extraction)? Some doctors have already specialized in performing FUE alone, so their opinion is already made up. Some doctors new to the business entered the FUE market having never done an FUT strip procedure. That means that the nuances of quality control have not been learned (tricks to prevent graft damage from manipulation and drying).
There is a question arising out of the hair transplant community which is becoming polarized and lining up for a fight: Which is better, FUT (Follicular Unit Transplant with Strip) or FUE (Follicular Unit Extraction)? Some doctors have already specialized in performing FUE alone, so their opinion is already made up. Some doctors new to the business entered the FUE market having never done an FUT strip procedure. That means that the nuances of quality control have not been learned (tricks to prevent graft damage from manipulation and drying). The long term results with FUE (particularly on donor area damage in extensive FUE grafting) is not yet in. When
The long term results with FUE (particularly on donor area damage in extensive FUE grafting) is not yet in. When