Snippet from the article:
In the dozen years since the Da Vinci robot has been approved for surgeries in the United States, it’s been embraced by health care providers and patients alike. Surgeons routinely use the multi-armed metal assistant to remove cancerous prostate glands and uteruses, repair heart valves and perform gastric bypass operations, among many other procedures.
Read the rest at Kaiser Health News — Questions Arise About Robotic Surgery’s Cost, Effectiveness
Although this article reflects upon robots used for abdominal, prostate, cardiac surgery, etc… some of the questions asked will apply to the ARTAS robotic hair transplant FUE system. More from the article: “At this time, health insurers generally pay for robotic surgery just as they would any other surgical procedure, and patient out-of-pocket costs are typically no different either. That could change, some say, as more comprehensive data become available that clarifies when robotic-assisted surgery helps improve patient outcomes—and when it doesn’t.”
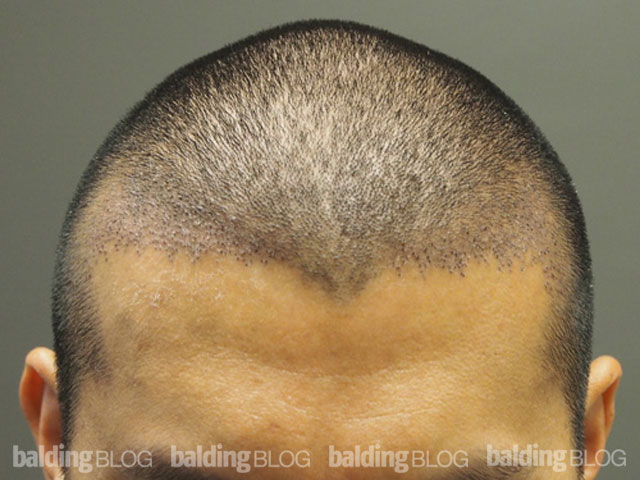
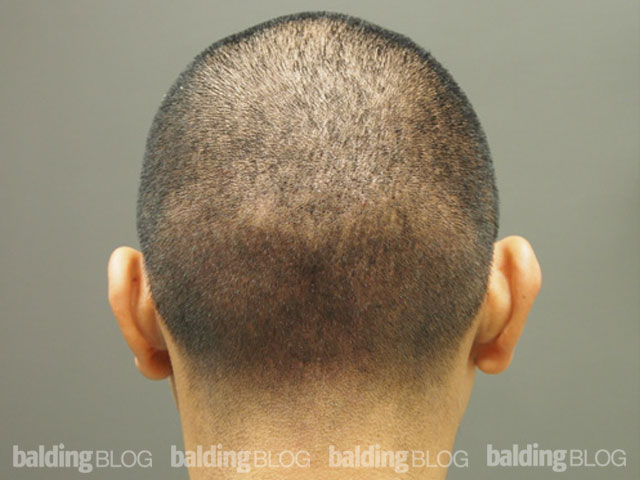
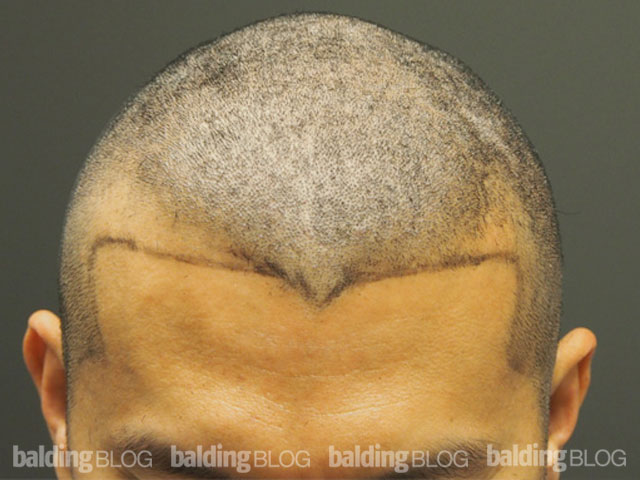
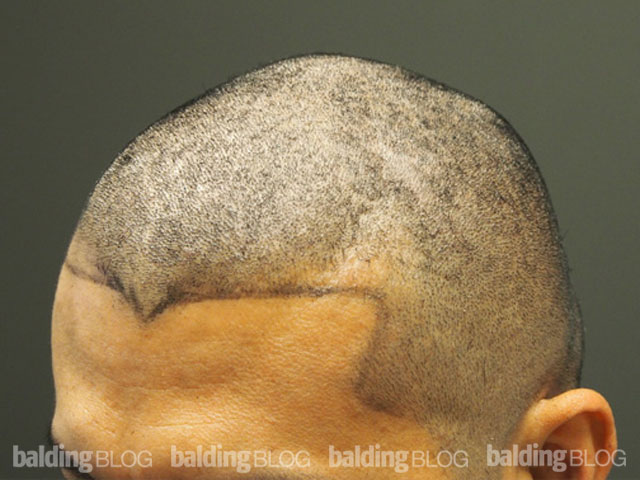
Robotic FUE with the ARTAS system does what appears to be an excellent job at the FUE itself; however, as the grafts that are created are removed manually, stored in traditional solutions, and placed manually, defects in process that were present before the robot was used will continue even with efficient drilling of the grafts.
“Robot-assisted surgeries are generally more expensive than other methods, however, and don’t necessarily improve patient outcomes long-term,” says the article. Although this statement is not referring to the FUE robot, the message is clear. What is it that the public is buying and what will the long term results actually be for the FUE robots?
Many of the ARTAS systems that have been sold to date were purchased by experienced hair restoration surgeons, so I suspect in their hands, the long term results will be good for them; however, for the novice doctor or the doctor who has not put together the system of people skills behind the robot for moving, storing, and placing the grafts, an imbalance in long term results may result. It will be years before we know, though.
Tags: artas®, fue, hair transplant, robot surgery, kaiser, hairloss, hair loss